Deep Vein Thrombosis (DVT)
https://my.clevelandclinic.org/
Management and Treatment
Activity Guidelines
You should slowly return to your normal activities. If your legs feel swollen or heavy, lie in bed with your heels propped up about 5 to 6 inches. This helps improve circulation and decreases swelling.
In addition:
- Exercise your lower leg muscles if you are sitting still for long periods of time.
- Stand up and walk for a few minutes every hour while awake.
- Don’t wear tight-fitting clothing that could decrease the circulation in your legs.
- Wear compression stockings as recommended by your doctor.
- Avoid activities that may cause a serious injury.
compression stockings and elevating the affected leg. If the blood clot is extensive, you may need more invasive testing and treatment. The main goals of treatment are to:
- Stop the clot from getting bigger
- Prevent the clot from breaking off in your vein and moving to your lungs
- Reduce the risk of another blood clot
- Prevent long-term complications from the blood clot (chronic venous insufficiency).
Medications
- Have blood tests as directed by your doctor and keep all scheduled laboratory appointments.
- Do not stop or start taking any medication (including nonprescription/over-the-counter medications and supplements) without asking your doctor.
- diet. You may need to make changes, depending on the medication you take.
Treatment for a DVT can include:
Anticoagulants ("blood thinners"). This type of medication makes it harder for your blood to clot. Anticoagulants also stop clots from getting bigger and prevent blood clots from moving. Anticoagulants do not destroy clots. Your body may naturally dissolve a clot, but sometimes clots do not completely disappear.
There are different types of anticoagulants
If you need to take an anticoagulant, you may only need to take it for 3 to 6 months. But, your treatment time may be different if:
- You have had clots before, your treatment time may be longer.
- You are being treated for another illness (such as cancer), you may need to take an anticoagulant as long as your risk of a clot is higher.
The most common side effect of anticoagulants is bleeding. You should call your doctor right away if you notice that you bruise or bleed easily while taking this medication.
Compression Stockings
wear graduated compression stockings to get rid of leg swelling. The swelling is often because the valves in the leg veins are damaged or the vein is blocked by the DVT.Most compression stockings are worn just below the knee.
These stockings are tight at the ankle and become more loose as they go up the leg. This causes gentle pressure (compression) on your leg.
DVT Treatment Procedures
Vena cava filters are used when you cannot take medications to thin your blood or if you have blood clots while taking this type of medication. The filter prevents blood clots from moving from the vein in your legs to the lung (pulmonary embolism). The filter is put in place during minor surgery.
It is inserted through a catheter into a large vein in the groin or neck, then into the vena cava (the largest vein in the body). Once in place, the filter catches clots as they move through the body. This treatment helps prevent a pulmonary embolism, but does not prevent the formation of more clots.
+++++++++++
How is DVT diagnosed?
A duplex venous ultrasound. This is the most common test used to diagnose a DVT. It shows the blood flow in the veins and any blood clots that exist. An ultrasound technician will apply pressure while scanning your arm or leg. If the pressure does not cause the vein to compress, it could mean there is a blood clot.
Venography. This test uses X-rays to show your deep veins. A special dye (contrast material) is injected into your veins so the X-rays show the veins and any blood clots. Any blockage in blood flow may also be seen. Venography may be used if the results of the duplex ultrasound aren’t clear.
Other tests you may have include:
- Magnetic Resonance Imaging (MRI) or Magnetic Resonance Venography (MRV): MRI shows pictures of organs and structures inside the body, and MRV shows pictures of the blood vessels in the body. In many cases, MRI and MRV can offer more information than an X-ray.
- Computed tomography (CT) scan is a type of X-ray that shows structures inside the body. A CT scan may be used to find a DVT in the abdomen or pelvis, as well as blood clots in the lung (pulmonary embolism).
If your doctor thinks you may have a genetic disorder that causes blood clots, you may need blood tests. This may be important if:
- You have a history of blood clots that cannot be linked to any other cause
- You have a blood clot in an unusual location, such as in a vein from the intestines, liver, kidney or brain
- You have a strong family history of blood clots
++++++
Can a DVT be prevented?
to reduce your risk of future clots by:
- Taking your medications exactly as your doctor tells you to.
- Keeping your follow-up appointments with your doctor and the laboratory. These are needed to see how well your treatment is working.
- Exercise your lower leg muscles if you need to sit still for a long time. Stand up and walk at least every half hour if you are on a long flight. Or get out of the car every hour if you are on a long road trip.
- Get out of bed and move around as soon as you can after you are sick or have surgery. The sooner you move around, the less chance you have of developing a clot.
- Take medications or use compression stockings after surgery (if prescribed by your doctor) to reduce your risk of a clot.
- Follow-up with your doctor as directed to and follow your doctor’s recommendations to reduce your risk of a clot.
+++++++++++++
www.mayoclinic.org
Treatment
Deep vein thrombosis (DVT) treatment is aimed at preventing the clot from getting bigger and preventing it from breaking loose and causing a pulmonary embolism. Then the goal becomes reducing your chances of deep vein thrombosis happening again.
Blood thinners
drugs, which can be injected or taken as pills, decrease your blood's ability to clot. They don't break up existing blood clots, but they can prevent clots from getting bigger and reduce your risk of developing more clots.
Heparin is typically given intravenously. Other similar blood thinners, such as enoxaparin (Lovenox), dalteparin (Fragmin) or fondaparinux (Arixtra), are injected under the skin.
You might receive an injectable blood thinner for a few days, after which pills such as warfarin (Coumadin, Jantoven) or dabigatran (Pradaxa) are started. Once warfarin has thinned your blood, the injectable blood thinners are stopped.
Other blood thinners can be given in pill form without the need for an injectable blood thinner. These include rivaroxaban (Xarelto), apixaban (Eliquis) or edoxaban (Savaysa).
You might need to take blood thinner pills for three months or longer. It's important to take them exactly as your doctor instructs because taking too much or too little can cause serious side effects.
Lifestyle and home remedies
watch your diet and watch for signs of excessive bleeding, as well as take steps to prevent another DVT. Some things you can do include:
- Check in with your doctor regularly to see if your treatment needs to be modified. If you're taking warfarin (Coumadin, Jantoven), you'll need a blood test to see how well your blood is clotting.
- Take your blood thinners as directed. If you've had DVT, you'll be on blood thinners for at least three to six months.
- Watch for excessive bleeding, which can be a side effect of taking blood thinners. Talk to your doctor about activities that could cause you to bruise or get cut, as even a minor injury could become serious if you're taking blood thinners.
- Move. If you've been on bed rest because of surgery or other factors, the sooner you get moving, the less likely blood clots will develop.
- Wear compression stockings to help prevent blood clots in the legs if your doctor recommends them.
Preparing for your appointment
Deep vein thrombosis (DVT) is considered a medical emergency, so it's important to get evaluated quickly. However, if you have time before your appointment, here's some information to help you get ready.
questions to ask your doctor include:
- What's the most likely cause of my symptoms?
- What tests do I need?
- What's the best treatment?
- What are the alternatives to the primary approach that you're suggesting?
- Will I need to restrict my physical activity or travel?
- I have other health conditions. How can I best manage these conditions together?
- Are there brochures or other printed material I can have? What websites do you recommend?
If you develop signs or symptoms of a pulmonary embolism — a life-threatening complication of deep vein thrombosis — seek immediate medical attention.
The warning signs and symptoms of a pulmonary embolism include:
- Sudden shortness of breath
- Chest pain or discomfort that worsens when you take a deep breath or when you cough
- Feeling lightheaded or dizzy, or fainting
- Rapid pulse
- Coughing up blood
Risk factors
Prolonged bed rest, such as during a long hospital stay, or paralysis. When your legs remain still for long periods, your calf muscles don't contract to help blood circulate, which can increase the risk of blood clots.
Heart failure. This increases your risk of DVT and pulmonary embolism. Because people with heart failure have limited heart and lung function, the symptoms caused by even a small pulmonary embolism are more noticeable.
- Age. Being older than 60 increases your risk of DVT, though it can occur at any age.
- Sitting for long periods of time, such as when driving or flying. When your legs remain still for hours, your calf muscles don't contract, which normally helps blood circulate. Blood clots can form in the calves of your legs if your calf muscles don't move for long periods.
Complications
A serious complication associated with deep vein thrombosis is pulmonary embolism.
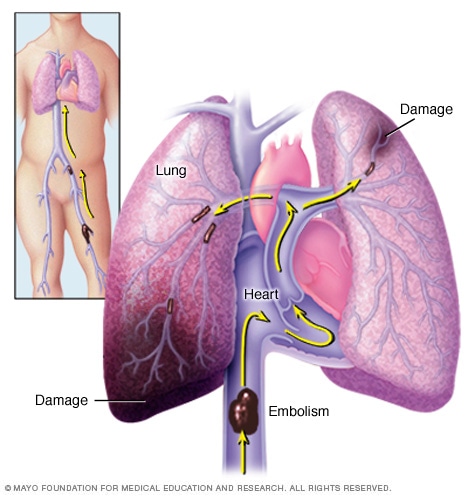
Pulmonary embolism occurs when a blood clot gets lodged in an artery in the lung, blocking blood flow to part of the lung. Blood clots most often originate in the legs and travel up through the right side of the heart and into the lungs.
A pulmonary embolism occurs when a blood vessel in your lung becomes blocked by a blood clot (thrombus) that travels to your lung from another part of your body, usually your leg.
A pulmonary embolism can be life-threatening. It's important to watch for signs and symptoms of a pulmonary embolism and seek medical attention if they occur. Signs and symptoms of a pulmonary embolism include:
- Sudden shortness of breath
- Chest pain or discomfort that worsens when you take a deep breath or when you cough
- Feeling lightheaded or dizzy, or fainting
- Rapid pulse
- Coughing up blood
Postphlebitic syndrome
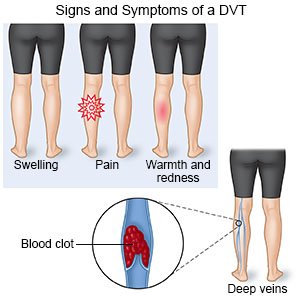
A common complication that can occur after deep vein thrombosis is known as postphlebitic syndrome, also called postthrombotic syndrome. Damage to your veins from the blood clot reduces blood flow in the affected areas, which can cause:
- Persistent swelling of your legs (edema)
- Leg pain
- Skin discoloration
- Skin sores
Prevention
Avoid sitting still. If you have had surgery or have been on bed rest for other reasons, try to get moving as soon as possible. If you're sitting for a while, don't cross your legs, which can hamper blood flow. If you're traveling a long distance by car, stop every hour or so and walk around.
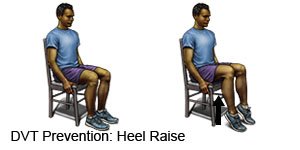
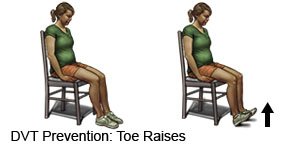
If you're on a plane, stand or walk occasionally. If you can't do that, exercise your lower legs. Try raising and lowering your heels while keeping your toes on the floor, then raising your toes with your heels are on the floor.
Exercise. Regular exercise lowers your risk of blood clots, which is especially important for people who sit a lot or travel frequently.
++++++++++++
www.webmd.com
How to Prevent Deep Vein Thrombosis (DVT)
- Lose weight.
- Exercise.
- Don’t stay still for long periods -- move every 2 hours or so when you’re on a plane or long car trip.
- Wear loose clothes and drink lots of water when you travel.
Check your blood pressureat least once a year; more often if your doctor says to. Follow his instructions about taking medication if you need it. Exercise, eating well, and quitting smoking will help control your blood pressure, too.
After Surgery or While on Bed Rest
Your doctor may prescribe blood thinners, also called anticoagulants:
- Apixaban (Eliquis)
- Betrixaban (Bevyxxa)
- Dabigatran (Pradaxa)
- Edoxaban (Savaysa)
- Fondaparinux (Arixtra)
- Heparin
- Rivaroxaban (Xarelto)
- Warfarin (Coumadin)
+++++++++++
www.nhs.uk
You have symptoms of DVT, such as pain and swelling and:
- breathlessness
- chest pain
DVT can be very serious because blood clots in your veins can break loose, travel through your bloodstream and get stuck in your lungs. This is called a pulmonary embolism.
A pulmonary embolism can be life threatening and needs treatment straight away.
A DVT is more likely to happen if you:
- are over 60
- are overweight
- smoke
- have had DVT before
- take the contraceptive pill or HRT
- have cancer or heart failure
- have varicose veins
Treatment of DVT
After DVT is diagnosed, the main treatment is tablets of an anticoagulant medicine, such as warfarin and rivaroxaban. You will probably take the tablets for at least 3 months.
Some lifestyle measures will help you recover from DVT.
After you leave hospital, you will be encouraged to:
- walk regularly
- keep your affected leg raised when you're sitting
- delay any flights or long journeys until at least 2 weeks after you start anticoagulant medicine
stay a healthy weight
stay active – taking regular walks can help
drink plenty of fluids to avoid dehydration – DVT is more likely if you're dehydrated
do not sit still for long periods of time – get up and move around every hour or so
do not cross your legs while you're sitting, it can restrict blood flow
++++++++++++
www.drugs.com
Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising while you take blood thinners. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines unless your healthcare provider tells you to. Many medicines cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip does or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
Warfarin is a blood thinner that you may need to take. The following are things you should be aware of if you take warfarin:
- Foods and medicines can affect the amount of warfarin in your blood. Do not make major changes to your diet while you take warfarin. Warfarin works best when you eat about the same amount of vitamin K every day. Vitamin K is found in green leafy vegetables and certain other foods. Ask for more information about what to eat when you are taking warfarin.
These tests are used to decide how much medicine you need.
- Clot busters are emergency medicines that work to dissolve blood clots.
- A vena cava filter may be placed inside your vena cava to treat your DVT. The vena cava is a large vein that brings blood from your lower body up to your heart. The filter may help trap pieces of a blood clot and prevent them from going into your lungs.
- Surgery called a thrombectomy may be done to remove the clot. A procedure called thrombolysis may instead be done to inject a clot buster that helps break the clot apart.
- Tissue plasminogen activator (tPA)
- Tenecteplase
- Alteplase
- Urokinase
- Reteplase
- Streptokin
Wear pressure stockings as directed. The stockings put pressure on your legs. This improves blood flow and helps prevent clots. Wear the stockings during the day. Do not wear them when you sleep.
Elevate your legs above the level of your heart. Elevate your legs when you sit or lie down, as often as you can. This will help decrease swelling and pain. Prop your legs on pillows or blankets to keep them elevated comfortably.


Prevent a DVT:
- Exercise regularly to help increase your blood flow. Walking is a good low-impact exercise. Talk to your healthcare provider about the best exercise plan for you.
Change your body position or move around often. Move and stretch in your seat several times each hour if you travel by car or work at a desk. In an airplane, get up and walk every hour. Move your legs by tightening and releasing your leg muscles while sitting. You can move your legs while sitting by raising and lowering your heels. Keep your toes on the floor while you do this. You can also raise and lower your toes while keeping your heels on the floor.
Maintain a healthy weight. Ask your healthcare provider how much you should weigh. Ask him or her to help you create a weight loss plan if you are overweight.
++++++++++++++
www.rochesterregional.org
Deep Vein Thrombosis
It is a very serious condition that can cause permanent damage to the leg, known as post-thrombotic syndrome, or a life-threatening pulmonary embolism
Recently, it has been referred to as “Economy Class Syndrome” due to the occurrence after sitting on long flights. افتكرت قبل يوم الحادثة العربية بابا اشتكي ليا قلة النوم وقبل سفر ابراهيم شكلة ومش عاوز اروح رجليه تعباه
life-threatening pulmonary embolism by blocking the oxygen supply, causing heart failure
Blood Thinners
Contrary to popular belief, blood thinners (anticoagulants) do not actively dissolve the clot, but instead prevent new clots from forming. Over time, the body will dissolve the clot, but often the vein becomes damaged in the meantime.
Post-thrombotic syndrome is an under-recognized, but relatively common aftereffect of DVT, where patients develop irreversible damage in the affected leg veins and their valves, resulting in abnormal pooling of blood in the leg, chronic leg pain, fatigue, swelling, and in extreme cases, severe skin ulcers. To prevent permanent leg damage, patients can receive catheter-directed thrombolysis treatment.
++++++++++++++
www.healthline.com
Tips for Managing Deep Vein Thrombosis at Home
occur anywhere in the body, but most often forms in the calf or thigh.
Treating DVT is important because of the risk of a life-threatening complication known as pulmonary embolism. This occurs when the blood clot breaks off and travels through the blood and blocks an artery in the lung.
Once you receive a diagnosis of DVT, you’ll likely be prescribed medications known as anticoagulants, or blood thinners. These work to keep the clot from growing and to prevent further clots. Research shows that taking these medications at home is just as safe and effective as taking them while in the hospital.
The main focus of DVT treatment at home includes:
- taking your prescribed anticoagulant medicine safely
- relieving symptoms, such as leg pain and swelling
- lifestyle changes to reduce your risk of another blood clot forming
take the anticoagulant medication for three to six months, sometimes longer.
Taking too much of an anticoagulant medication like warfarin can thin the blood too much and lead to bleeding problems.
To avoid bleeding problems, you can follow these steps:
- Prevent injuries or falls, which include avoiding contact sports, wearing protective gear like a helmet, or using a walker or cane.
- Inform your doctors about any other medications, supplements, and vitamins you’re taking.
- Visit your doctor for regular partial thromboplastin time (PTT) tests to make sure you’re receiving the right dose of anticoagulant if your doctor tells you to do so.
- Avoid changing or stopping your medication unless your doctor tells you to.
- Take your medication at the same time each day.
- Call your doctor if you miss a dose.
- Make sure all your doctors and dentists know you’re on anticoagulants.
- Eat a balanced diet
To ease the pain and swelling of a DVT, you can try the following at home:
- Wear graduated compression stockings. These specially fitted stockings are tight at the feet and become gradually looser up on the leg, creating gentle pressure that keeps blood from pooling and clotting.
Elevate the affected leg. Make sure your foot is higher than your hip.
Take walks. Aim for walks three to five times a day to improve blood flow to your legs.
If you’ve been prescribed anticoagulant medications, don’t take aspirin and medications that contain aspirin. Avoid other nonsteroidal anti-inflammatory drugs (NSAIDs) as well. These include ibuprofen (Advil, Motrin) and naproxen (Aleve).
These lifestyle changes can help prevent DVT:
- Quit smoking.
- Lower your blood pressure with dietary changes, like reducing your salt and sugar intake.
- Lose weight if you’re overweight.
- Avoid sitting for long periods of time. Get up and walk around every so often if you’re driving or on a long flight. Flex your feet to stretch out your calves.
- Exercise, such as walking or swimming, every day.
- Don’t wear tight clothing when traveling long distances.
- Wear graduated compression stockings, especially after a surgery or if you’re on bed rest.
- Drink lots of fluids.
- Stop taking birth control pills prior to surgery, if directed by a doctor.
Ginger الزنجبيل
Ginger may help prevent DVT because it contains an acid called salicylate. Acetyl salicylic acid, which is derived from salicylate and is commonly known as aspirin, is used to prevent stroke. Ginger is a common ingredient in many recipes. It can also be made into a tea. Ginger has many other health benefits as well.
Turmeric الكركم
A compound in turmeric called curcumin is responsible for its blood-thinning properties. Curcumin may help improve the function of the endothelium, or the lining of the blood vessels, and improve its ability to regulate blood pressure and blood clotting.
You can use turmeric as a spice in any recipe, or try it in a drink with milk and honey. It’s also available in supplement and extract form.
Cayenne pepper فلفل حريق
Cayenne peppers contain high amounts of salicylates. They may help lower blood pressure, thin the blood, and increase circulation. Cayenne peppers can be added to your cooking whole, or they can be ground up into a powder. If spicy food isn’t your thing, you can take cayenne pepper supplements in capsule form.
Vitamin E
Foods high in vitamin E are natural blood thinners. You can find vitamin E in olive, corn, and soybean oils. Other vitamin E-rich foods include greens like spinach and kale, kiwi, almonds, tomato, mango, and broccoli.
Don’t eat very large amounts of leafy green vegetables if you’re taking warfarin. Leafy green vegetables contain vitamin K. Too much vitamin K can lower the effect of warfarin.
Omega-3 fatty acids
Omega-3 fatty acids may help lower blood pressure and reduce cholesterol, triglycerides, and inflammation. All of these play a role in preventing blood clots. You can find omega-3s in fish or fish oil supplements.
Remember that certain herbal supplements and vitamins shouldn’t be taken with your anticoagulant medication. Seek immediate medical attention if you notice any signs of abnormal bleeding due to your anticoagulant medication, including:
- coughing or vomiting blood
- blood in the stool or urine
- a nosebleed that doesn’t stop
- bruises that form without a known cause
+++++++++++
How to Tell If You Have a Blood Clot 2017
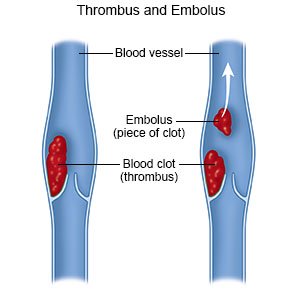
When a clot forms inside one of your veins, it won’t always dissolve on its own. This can be a very dangerous and even life-threatening situation.
An immobile blood clot generally won’t harm you, but there’s a chance that it could move and become dangerous. If a blood clot breaks free and travels through your veins to your heart and lungs, it can get stuck and prevent blood flow. This is a medical emergency.
A healthcare professional will be able to look at your symptoms and medical history and let you know what steps to take from there.
requires emergency treatment. The symptoms of an arterial clot include severe pain, paralysis of parts of the body, or both. It can lead to a heart attack or stroke.
may build up more slowly over time, but they can still be life-threatening. The most serious type of venous clot is called deep vein thrombosis.
Deep vein thrombosis (DVT) is the name for when a clot forms in one of the major veins deep inside your body. It’s most common for this to happen in one of your legs, but it can also happen in your arms, pelvis, lungs, or even your brain.
تعليقات
إرسال تعليق